
The Role of Interdental Cleaning for Oral Health, General Health and Quality of Life
Recent research shows that oral health is an essential prerequisite for people’s well-being and quality of life. In order to reach the global goals for oral health, the dental profession has a great responsibility to work with a preventive and health-promoting approach.
Oral health is multi-faceted and includes the ability to speak, smile, taste, touch, chew, swallow and convey a range of emotions through facial expressions with confidence and without pain, discomfort and disease of the craniofacial complex, according to the definition from the World Dental Federation, FDI (Glick et al. 2016). With this definition in mind, oral health is an undeniable part of general health and wellbeing.
The Broad Consequences of Oral Disease
Periodontal disease is common worldwide. It affects approximately 50% of the adult population, and severe periodontitis prevalence varies from 10 to 15%; prevalence figures are positively associated with increasing age (Chapple et al. 2015, Petersen and Ogawa 2012, Eke et al. 2015). Given the massive effects of the disease, it becomes clear that it should be a matter of global concern.
First, there is growing scientific support for a link between periodontal disease and several general diseases, e.g., cardiovascular disease, diabetes, and obesity. Thus, oral diseases are no longer considered as local problems affecting the oral cavity but rather diseases with consequences for overall health (Holmstrup et al. 2017).
Research has also shown a significant association between periodontal disease and oral health-related quality of life – independent of factors like age, gender and other dental problems (Masood et al. 2019). The disease can contribute to anxiety, low self-esteem, and feelings of shame and vulnerability (Herrera et al.).
Oral diseases also have a vast impact from a financial perspective. In 2015, on a global basis, the total cost was shown to be $544.41 billion, where direct costs, measured as dental expenditures costs, accounted for $356.80 billion, and indirect costs, measured as productivity losses, were $187.61 billion. Among oral diseases, periodontitis was the second biggest cause for global productivity costs (Righolt et al. 2018). Severe periodontitis accounts for $54 billion yearly due to indirect costs (Listl et al. 2015).
Causes and Prevention
Dental professionals have a central role in preventing disease through a health-promoting approach based on science and proven clinical experience. Evaluating individual needs and conditions and weighing them together with scientific support should form the basis for instructions and recommendations, thus creating the best possible foundation for patient compliance and long-lasting oral health.
There are several risk factors for the development of periodontitis. Most important is the accumulation of a plaque biofilm along and below the gingival margin. Control and removal of this biofilm are of utmost importance to maintain oral health. The significance of good oral hygiene in order to prevent oral disease is, therefore, indisputable.
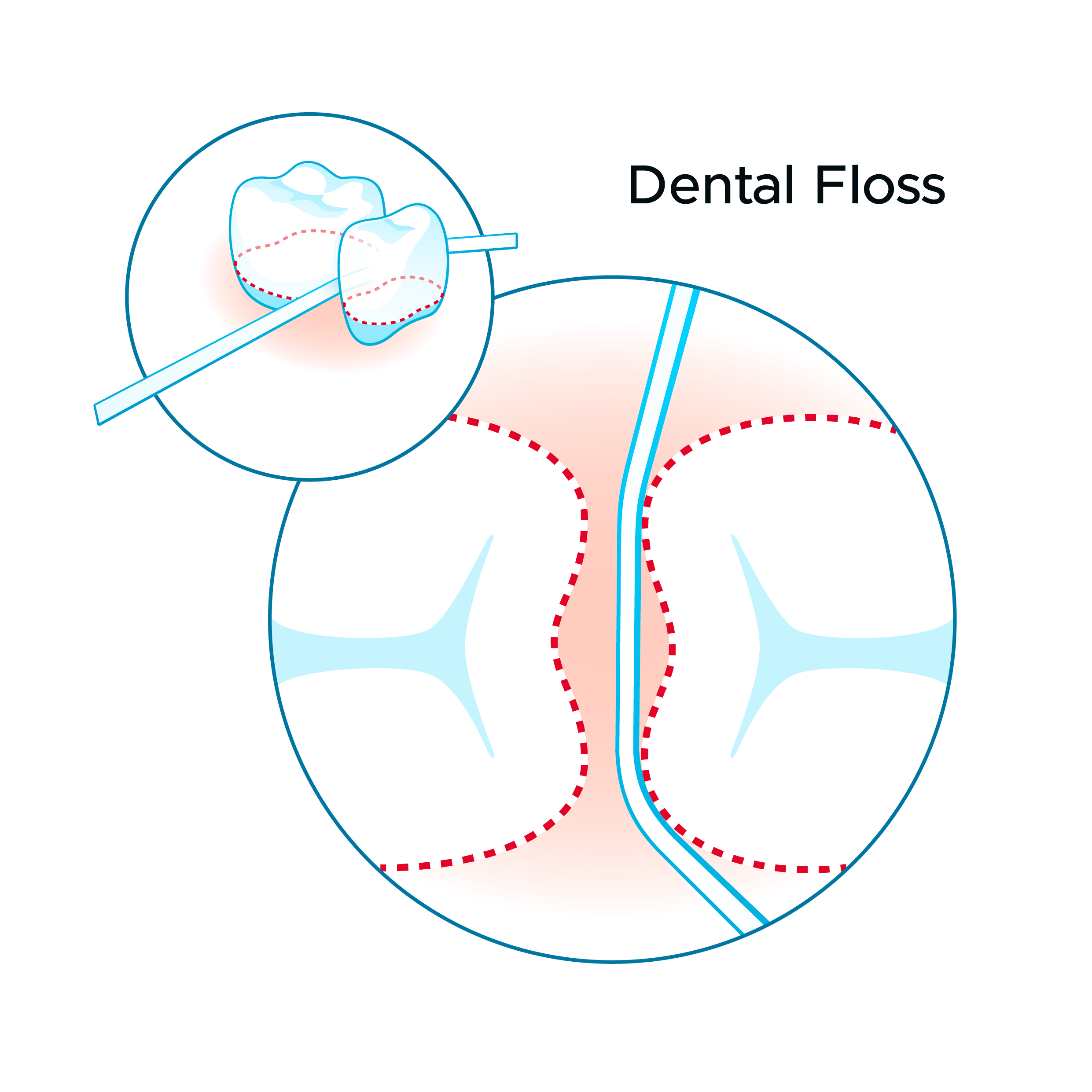
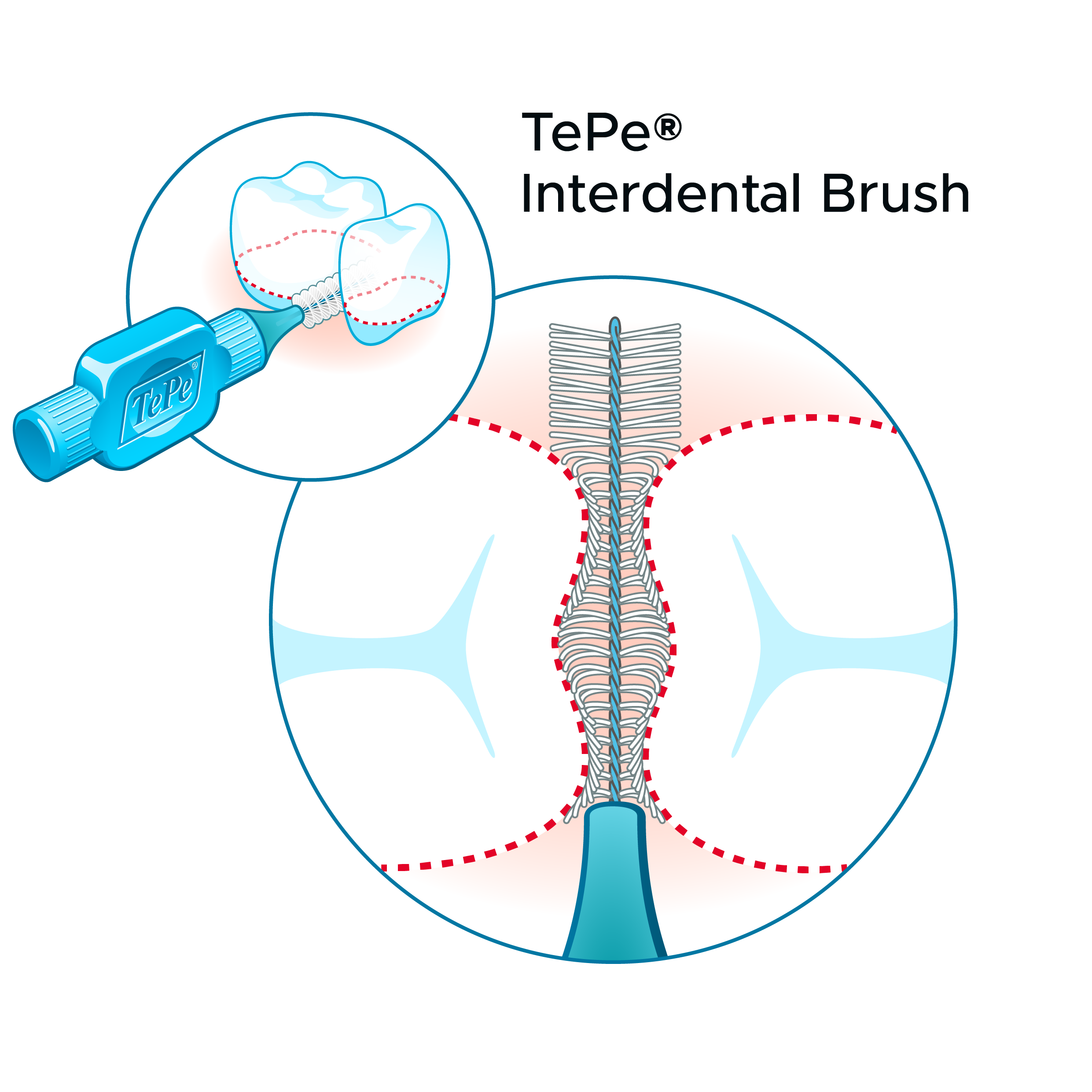
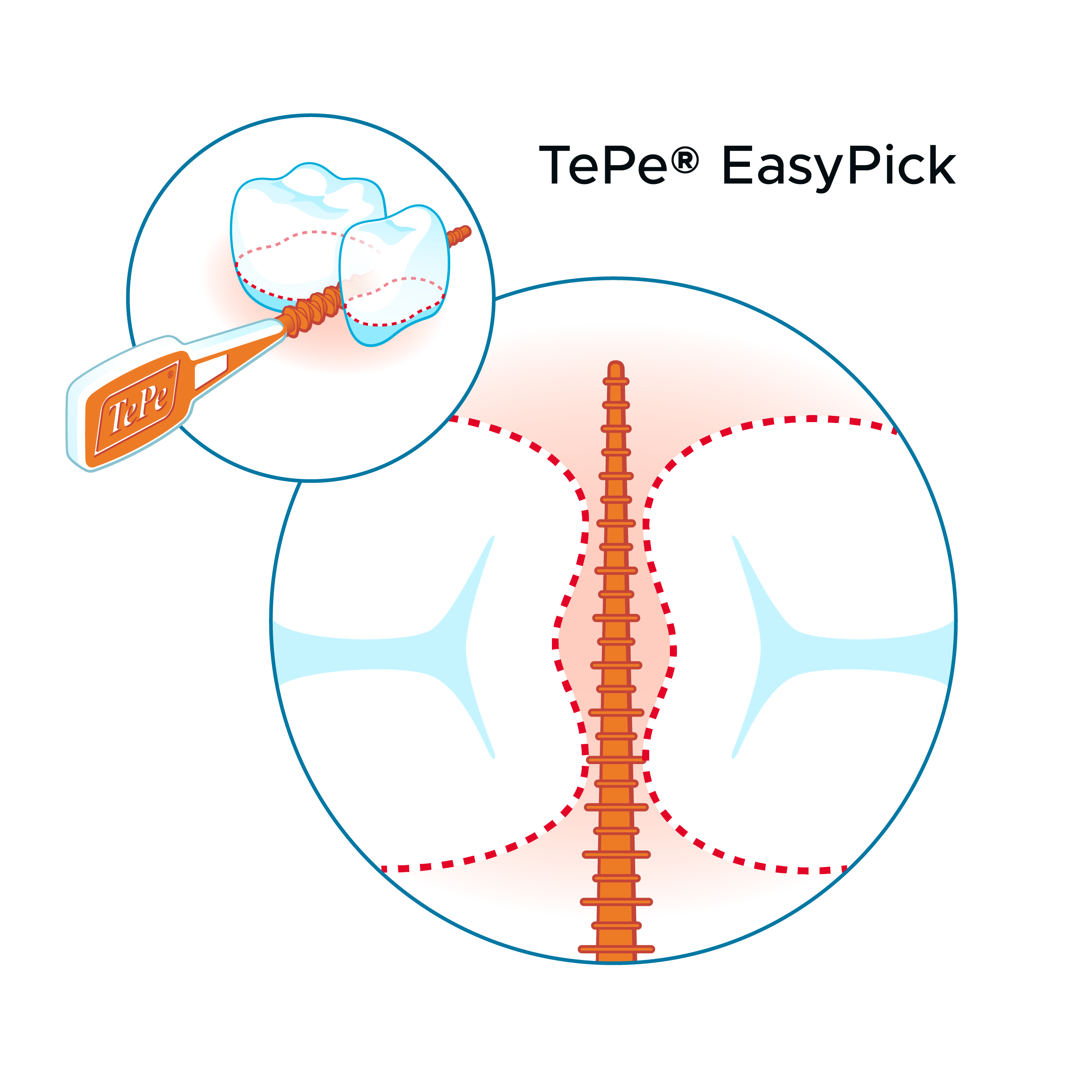
Toothbrushing and interdental cleaning are cornerstones to achieve high-quality oral hygiene. Interdental cleaning is associated with lower levels of periodontal disease, and periodontal health increases with a higher frequency of use of interdental cleaning devices (Marchesan et al. 2018). The recommendation of an interdental cleaning device needs to be tailored, but for the majority of the grown-up population, an interdental brush is preferred.
A meta-review concluded that there is consistent evidence for interdental brushes being the most effective devices for interdental plaque removal (Sälzer et al. 2015).
This is also stated in the report of the 11th European Workshop in Periodontology on primary prevention of periodontitis (Chapple et al. 2015). According to the working group, interdental brushes are the preferred choice for interdental cleaning, while floss is an alternative only when sites are too narrow for the interdental brush and show gingival and periodontal health. These results were confirmed in a network metaanalysis where interdental brushes displayed the best result regarding gingival inflammation, plaque reduction and pocket reduction (Kotsakis et al. 2018).
From the presented articles, it appears that interdental brushes, when compared with other manual cleaning devices, have the highest efficacy in terms of plaque removal and periodontal parameters. Every recommendation regarding interdental cleaning devices must be tailored; the sizes and shapes of the interdental spaces must be considered. In addition, an individual who is recommended to use interdental brushes needs to be instructed regarding the appropriate size or sizes, and on an appropriate technique (Claydon 2008).
Conclusion
Current research emphasizes the importance of good oral hygiene in maintaining oral health and its consequences for general health and quality of life. Because the most common oral diseases are predominantly interdental diseases, preventive efforts must include interdental cleaning as an adjunct to toothbrushing in daily home care. In achieving optimal plaque control, the interdental brush is the preferred device for most of the adult population globally.
A preventive approach is well in line with the global goals for oral health 2020 from FDI, where one of the targets is to increase the population of people in all ages with healthy periodontium (Hobdell et al. 2003). FDI also has a vision for 2020 of ensuring that oral health is recognized and accepted as a core element of general health and wellbeing (Glick et al. 2012). In light of the financial reports, a preventive approach is most likely beneficial also from an economic perspective, since it will limit the need for other dental treatments.
REFERENCES
A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. Int Dent J. 2016 Dec;66(6):322-324.
Primary prevention of periodontitis: managing gingivitis. Chapple IL, Van der Weijden F, Doerfer C, Herrera D, Shapira L, Polak D, Madianos P, Louropoulou A, Machtei E, Donos N, Greenwell H, Van Winkelhoff AJ, Eren Kuru B, Arweiler N, Teughels W, Aimetti M, Molina A, Montero E, Graziani F. J Clin Periodontol. 2015 Apr;42 Suppl 16:S71-6.
The global burden of periodontal disease: towards integration with chronic disease prevention and control. Petersen PE, Ogawa H. Periodontol 2000. 2012 Oct;60(1):15- 39.
Update on Prevalence of Periodontitis in Adults in the United States: NHANES 2009 to 2012. Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, Borgnakke WS, Taylor GW, Page RC, Beck JD, Genco RJ. J Periodontol. 2015 May;86(5):611-22.
Comorbidity of periodontal disease: two sides of the same coin? An introduction for the clinician. Holmstrup P, Damgaard C, Olsen I, Klinge B, Flyvbjerg A, Nielsen CH, Hansen PR. J Oral Microbiol. 2017 Jun 14;9(1):1332710.
Relationship of periodontal disease and domains of Oral Health-related quality of life. Masood M, Younis LT, Masood Y, Bakri NN, Christian B. J Clin Periodontol. 2019 Jan 18. doi: 10.1111/jcpe.13072.
White Paper on Prevention and Management of Periodontal Diseases for Oral Health and General Health. Herrera D, Meyle J, Renvert S, Jin L. https://www.fdiworlddental.org/sites/default/files/media/resources/gphp-2018- white_paper-en.pdf Global-, Regional-, and Country-Level Economic Impacts of Dental Diseases in 2015.
Righolt AJ, Jevdjevic M, Marcenes W, Listl S. J Dent Res. 2018 May;97(5):501-507.
Global Economic Impact of Dental Diseases. Listl S, Galloway J, Mossey PA, Marcenes W. J Dent Res. 2015 Oct;94(10):1355-61. Interdental Cleaning Is Associated with Decreased Oral Disease Prevalence. Marchesan JT, Morelli T, Moss K, Preisser JS, Zandona AF, Offenbacher S, Beck J. J Dent Res. 2018 Jul;97(7):773-778.
Efficacy of inter-dental mechanical plaque control in managing gingivitis - a metareview. Sälzer S, Slot DE, Van der Weijden FA, Dörfer CE. J Clin Periodontol. 2015 Apr;42 Suppl 16:S92-105.
Primary prevention of periodontitis: managing gingivitis. Chapple IL, Van der Weijden F, Doerfer C, Herrera D, Shapira L, Polak D, Madianos P, Louropoulou A, Machtei E, Donos N, Greenwell H, Van Winkelhoff AJ, Eren Kuru B, Arweiler N, Teughels W, Aimetti M, Molina A, Montero E, Graziani F. J Clin Periodontol. 2015 Apr;42 Suppl 16:S71-6.
A network meta-analysis of interproximal oral hygiene methods in the reduction of clinical indices of inflammation. Kotsakis GA, Lian Q, Ioannou AL, Michalowicz BS, John MT, Chu H. J Periodontol. 2018 May;89(5):558-570. Current concepts in toothbrushing and interdental cleaning. Claydon NC. Periodontol 2000. 2008;48:10-22.
Global goals for oral health 2020. Hobdell M, Petersen PE, Clarkson J, Johnson N. Int Dent J. 2003 Oct;53(5):285-8.
About the Author

Anna Nilvéus Olofsson, DDS
Dr Anna Nilvéus Olofsson is manager of Odontology and Scientific Affairs at TePe.
Discover More
This article was originally published in the Clinical Life™ magazine: Spring 2023 edition
Clinical Life™ magazine is a premier periodical publication by Clinical Research Dental Supplies & Services Inc. Discover compelling clinical cases from Canadian and US dental professionals, cutting-edge techniques, product insights, and continuing education events.











