
Patient Management and Treatment of the Midline Diastema
A treatment plan is likely to be accepted by a patient if there is, at a minimum, a faith in the dentist that the restorative result will reflect the patient’s desired outcome at the agreed upon cost and timeline. This is especially true with a new patient with whom there is little or no shared dental experience. Any treatment plan requires a thorough investigation and assessment of clinical findings and is necessary to present treatment options and promote the patient’s understanding and ownership of their existing dental condition and its impact on the restorative result. There is a burden of responsibility to collect as much information from the patient as it relates to all aspects of treatment. However, this responsibility does not end with the clinical examination of hard and soft tissues, radiographs, photos, models, and medical history. Taking time to establish a rapport, delving into past dental experiences, and attempting to assess their potential as partners in the restorative process is essential to mitigate any challenges once treatment begins. Trust in the clinician can build as the case progresses, allowing the patient to “keep the faith”, as the patient’s ongoing engagement and cooperation can be critical to obtaining the desired clinical result.
Such was the case when a young woman presented as a new patient seeking options to improve the appearance of her “flat front teeth”. (FIG. 1)

FIG. 1
A young woman presented for treatment options to “fix her flat front teeth”. The accepted treatment plan involved short-term aligner therapy followed by a midline diastema closure and lengthening of the maxillary central incisors


FIG. 2A & 2B
Scans of the mandibular and maxillary arches were obtained. Models were made from these and mounted. Wax-ups of the ideal restorative result were then fabricated on these mounted models.

FIG. 3
The lingual matrix is replaced on the prepared teeth to verify its accuracy of fit. A lingual matrix, using Template Ultra Quick Matrix Material (Clinician’s Choice), was made from the wax-up. This allowed for the established, desired lingual contours and incisal edge locations to be accurately transferred to the preparations on teeth #8 and 9.

FIG. 4
Once the existing midline restorations were removed, a starburst bevel was established on the facial surfaces of teeth #8 and 9 using a F8888 (Brasseler) fine diamond bur. A short bevel was placed on the lingual of these teeth.

FIG. 5
A PrepStart air-abrasion system (Danville) was used on the facial and incisal to remove unwanted tooth and composite debris and aid in increasing the overall quality of the adhesive bond.

FIG. 6
With a mylar strip providing isolation from the adjacent teeth, the facial surface of the tooth was etched with 35% phosphoric acid beyond the starburst bevel, and carried over to the lingual surface, for a total of 20 seconds.

FIG. 7
Once the etch was thoroughly rinsed from the prepared tooth, a single layer of Adhese Universal adhesive (Ivoclar) was scrubbed onto the etched surface for 20 seconds, then air-thinned and light-cured

FIG. 8
Very thin layers of Evanesce Enamel White (Clinician's Choice) were placed in the incisal area of teeth #8 and 9 within lingual matrix and this matrix was replaced on the teeth. This layer was then attached to the preparation using a combination of an REJ #4 composite instrument (Clinician’s Choice) and a #3 composite brush lightly coated with ResinBlend LV (Clinician’s Choice). These lingual shells were light-cured in place.

FIG. 9
With a mylar strip separating tooth #9 from the adjacent teeth, Evanesce A1U (Clinician's Choice) was adapted to the mesial surface using an REJ #4 composite instrument. The pull-through technique was utilized to ensure an ideal proximal contour, natural contact area and emergence profile.
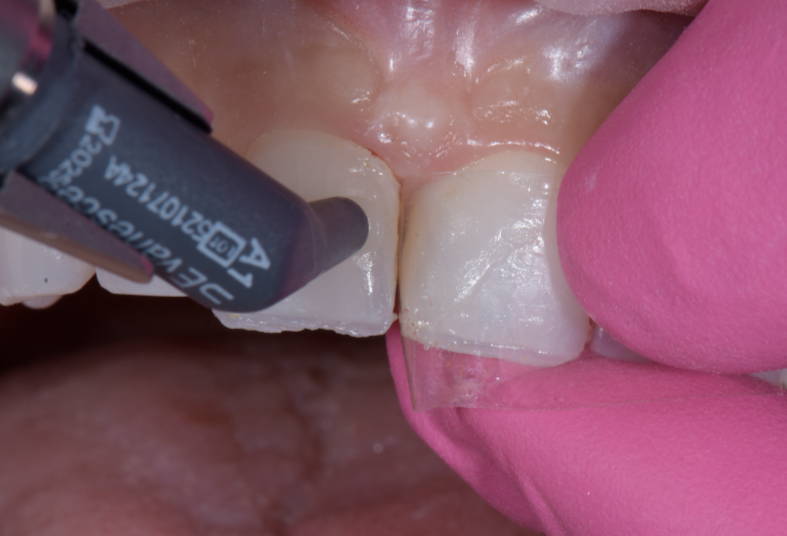
FIG. 10
The exact technique for placement and adaptation of Evanesce A1U composite was repeated on tooth #8 in order to close the midline diastema.
sequence of medium, fine and super-fine discs was followed to prepare the restorations for polishing. (FIG. 12)
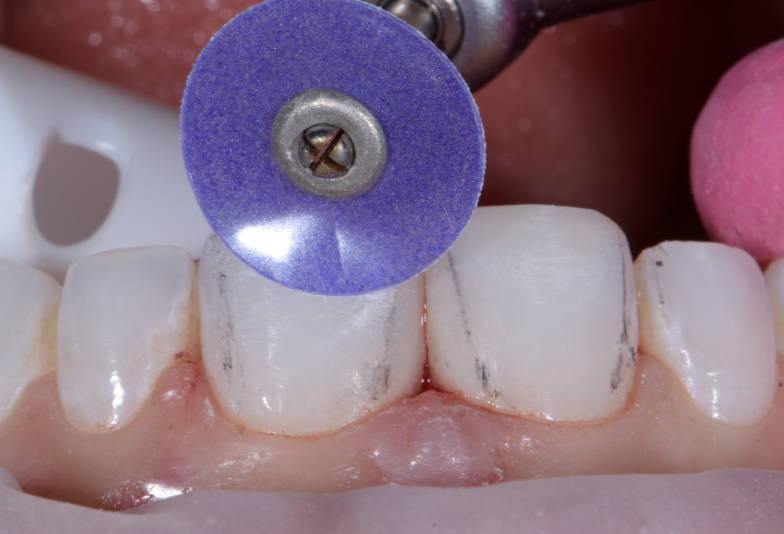
FIG. 11
Pencil lines drawn on the restored and adjacent teeth provide a visual guide to the placement of the proximal line angles. A coarse Contours Finishing and Polishing Disc (Clinician’s Choice) was used to “move” these line angles into their natural positions.

FIG. 12
Once the adjustments of the axial inclination, incisal length and location and proximal line angles have been made, the sequence of Contours Discs was followed from medium to fine to super-fine to prepare the restorative surfaces for the polishing steps.
Shine Cotton Polishing Wheel (Clinician’s Choice) with a light touch. (FIG. 14) The resulting restorations on teeth #8 and 9 were met with enthusiastic approval from the young patient. (FIG. 15)
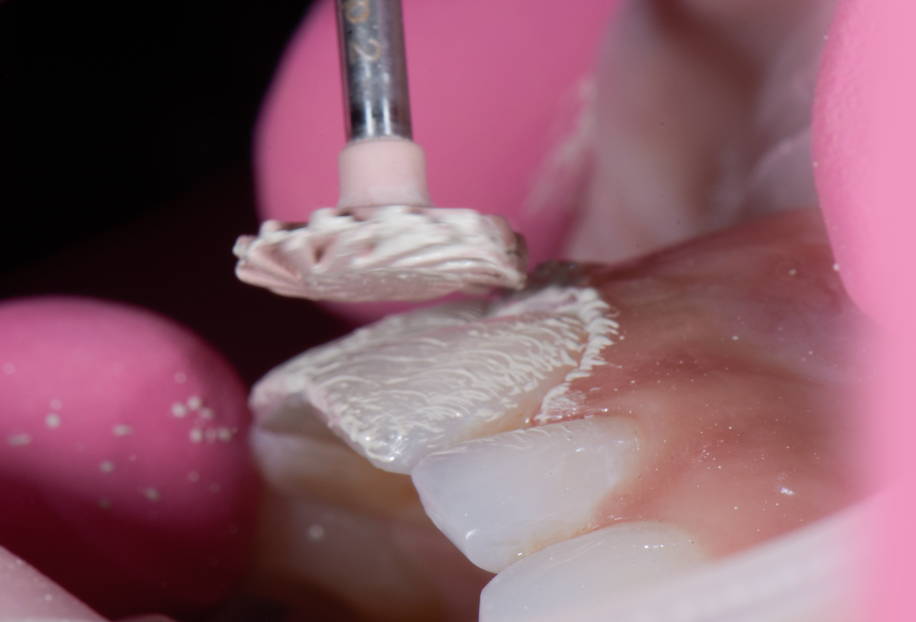
FIG. 13
The polishing of the Evanesce A1U composite to a high luster was completed using the A.S.A.P. 2-step diamond polishing system (Clinician’s Choice) in under 1 minute. The purple Pre-polisher was used at medium pressure for 15 to 20 seconds before switching over to the peach Final High Shine Polisher (seen here) for an additional 15-20 seconds under light pressure.

FIG. 14
In this case, the highest possible luster was required to match the surrounding dentition. A Final Shine Cotton Wheel (Clinician’s Choice) was used with a small amount of Enamelize polishing paste at low speed and low pressure to attain this.

FIG. 15
The resulting restorations on teeth #8 and 9 successfully reflected the patient’s esthetic expectations.

FIG. 16
The young patient was thrilled with her restorative results. While this case successfully met the expectations and goals of the treatment plan, it highlighted the need to maintain awareness of the patient’s motivation and participation as an integral contribution to achieving the clinical goal
About the Author

Dimple Desai, DDS, AAACD
Dr. Dimple Desai is the founder of Luminous Smiles of Newport Beach, a boutique dental practice focusing on rejuvenating patients’ lives through their smiles. She is one of the 350 Accredited Members of the American Academy of Cosmetic Dentistry in the world. Dr. Desai has been recognized locally as Orange County’s Top Dentist for the past four years and was selected as one of the Top 40 Dentists under the age of 40 in the country. Dr. Desai has been featured in various dental publications and continues to dedicate her passion to advancing her career in Dentistry. Dr. Desai is also a graduate of the Kois Institute and obtained both her Bachelor’s degree in Dental Hygiene and a Doctorate of Dental Surgery from the University of Southern California. She later returned to her Alma Mater as a Clinical Adjunct Professor to educate dental students on the clinic floor.
Discover More
This article was originally published in the Clinical Life™ magazine: Fall 2023 edition
Clinical Life™ magazine is a premier periodical publication by Clinical Research Dental Supplies & Services Inc. Discover compelling clinical cases from Canadian and US dental professionals, cutting-edge techniques, product insights, and continuing education events.
Subscribe to our emails to receive articles like this and be notified about our exclusive promotions.











